We call for a global moratorium on all clinical uses of human germline editing — that is, changing heritable DNA (in sperm, eggs or embryos) to make genetically modified children.
By ‘global moratorium’, we do not mean a permanent ban. Rather, we call for the establishment of an international framework in which nations, while retaining the right to make their own decisions, voluntarily commit to not approve any use of clinical germline editing unless certain conditions are met.
To begin with, there should be a fixed period during which no clinical uses of germline editing whatsoever are allowed. As well as allowing for discussions about the technical, scientific, medical, societal, ethical and moral issues that must be considered before germline editing is permitted, this period would provide time to establish an international framework.
Thereafter, nations may choose to follow separate paths. About 30 nations currently have legislation that directly or indirectly bars all clinical uses of germline editing1, and they might choose to continue the moratorium indefinitely or implement a permanent ban. However, any nation could also choose to allow specific applications of germline editing, provided that it first: gives public notice of its intention to consider the application and engages for a defined period in international consultation about the wisdom of doing so; determines through transparent evaluation that the application is justified; and ascertains that there is broad societal consensus in the nation about the appropriateness of the application. Nations might well choose different paths, but they would agree to proceed openly and with due respect to the opinions of humankind on an issue that will ultimately affect the entire species.
To be clear, our proposed moratorium does not apply to germline editing for research uses, provided that these studies do not involve the transfer of an embryo to a person’s uterus. It also does not apply to genome editing in human somatic (non-reproductive) cells to treat diseases, for which patients can provide informed consent and the DNA modifications are not heritable.
The 18 signatories of this call include scientists and ethicists who are citizens of 7 countries. Many of us have been involved in the gene-editing field by developing and applying the technology, organizing and speaking at international summits, serving on national advisory committees and studying the ethical issues raised.
Here, we lay out why we think such a moratorium is now warranted, and illustrate how an international framework might work.
The need
At the first International Summit on Human Gene Editing in December 2015, the organizing committee issued a statement about appropriate uses of the technology (see go.nature.com/2erqwpc). About the issue of making genetically modified children, it concluded that “it would be irresponsible to proceed with any clinical use … unless and until (i) the relevant safety and efficacy issues have been resolved … and (ii) there is broad societal consensus about the appropriateness of the proposed application”.
This should have been understood to mean that clinical uses of germline editing should not yet proceed anywhere in the world. Yet, subsequent events suggest that this statement was inadequate.
First, in China, biophysicist He Jiankui reportedly edited embryos to create at least two babies. Second, scientists who were apparently aware of this work did not take adequate measures to stop it. Third, there has been growing interest in proposals for genetic enhancement of humans2,3. Fourth, some commentators have interpreted subsequent statements as weakening the requirement for broad societal consensus4; such statements include a 2017 report from the US National Academies of Sciences, Engineering, and Medicine5 and a 2018 statement from the organizing committee following the Second International Summit on Human Genome Editing (see go.nature.com/2rowv3g). Finally, no mechanism was created in the ensuing years to ensure international dialogue about whether and, if so, when clinical germline editing might be appropriate.
A global moratorium and framework are therefore necessary to ensure proper consideration of the relevant issues surrounding clinical uses of germline editing.
Technical considerations. For germline editing to even be considered for a clinical application, its safety and efficacy must be sufficient — taking into account the unmet medical need, the risks and potential benefits and the existence of alternative approaches.
Although techniques have improved in the past several years, germline editing is not yet safe or effective enough to justify any use in the clinic. As was evident at the second summit, there is wide agreement in the scientific community that, for clinical germline editing, the risk of failing to make the desired change or of introducing unintended mutations (off-target effects) is still unacceptably high. Considerable research is being directed at this issue.
Scientific considerations. No clinical application of germline editing should be considered unless its long-term biological consequences are sufficiently understood — both for individuals and for the human species.
Among the vast array of possible genetic modifications, it is useful to distinguish between ‘genetic correction’ and ‘genetic enhancement’.
By genetic correction, we mean editing a rare mutation that has a high probability (penetrance) of causing a severe single-gene disease, with the aim of converting the mutation into the DNA sequence carried by most people. Assuming that it can be done without errors or off-target effects, genetic correction could have a predictable and beneficial effect.
Genetic enhancement, by contrast, encompasses much broader efforts to ‘improve’ individuals and the species. Possibilities range from attempting to modify the risk of a common disease by replacing particular genetic variants with alternative ones that occur in the human population, to incorporating new instructions into a person’s genome to enhance, say, their memory or muscles, or even to confer entirely new biological functions, such as the ability to see infrared light or break down certain toxins.
Understanding the effect of any proposed genetic enhancement will require extensive study — including of human population genetics and molecular physiology. Even so, substantial uncertainty would probably remain.
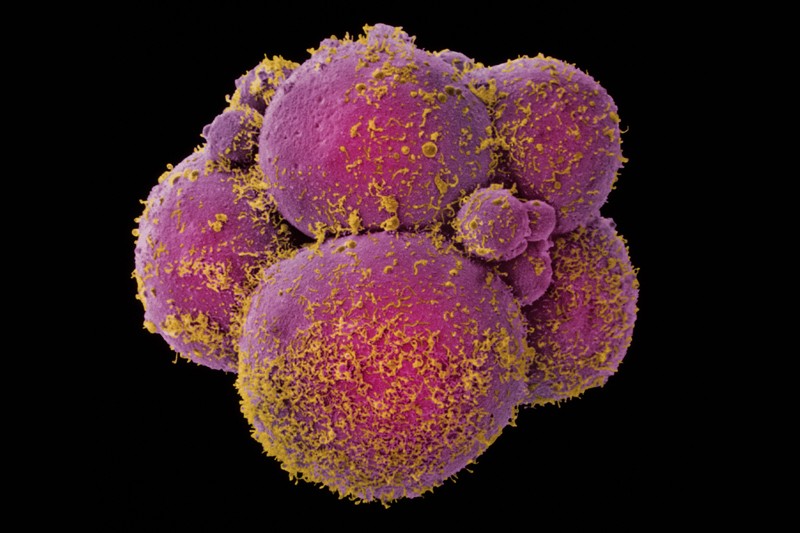
A human embryo at the eight-cell stage.Credit: Yorgos Nikas/SPL
Modifying disease risk by replacing genetic variants with alternative ones is fraught with challenges, because variants that decrease the risk of some diseases often increase the risk of others. A common variant in the gene SLC39A8, for instance, decreases a person’s risk of developing hypertension and Parkinson’s disease, but increases their risk of developing schizophrenia, Crohn’s disease and obesity6. Its influence on many other diseases — and its interactions with other genes and with the environment — remains unknown.
It will be much harder to predict the effects of completely new genetic instructions — let alone how multiple modifications will interact when they co-occur in future generations. Attempting to reshape the species on the basis of our current state of knowledge would be hubris.
The work of He illustrates this point. Seeking to decrease the children’s risk of acquiring AIDS if exposed to HIV later in life, He attempted to inactivate the gene CCR5, which encodes a receptor that HIV uses to enter cells. However, this change is not benign: it has been reported to substantially increase the risk of complications, and death, from certain other viral infections, including West Nile virus and influenza. It could have other consequences, too — both positive and negative (see Naturehttp://doi.org/gfphqv (2018) and ref. 7). As a societal solution to AIDS, disrupting CCR5 through clinical germline editing is ill-advised. Germline editing would not help individuals with the infection today, and it would require many decades of widespread use to make a dent in the epidemic. And, if an effective HIV vaccine is developed, the genetic enhancement would confer no benefit with respect to AIDS, yet still increase the risk of complications from other infections.
Full text: https://www.nature.com/articles/d41586-019-00726-5